Laboratories are steadily embracing digital pathology, even with the many challenges to widespread adoption. Digital pathology has the potential to transform pathology by improving efficiency, depth of analysis, and the opportunity for collaboration. By adopting a sophisticated anatomic pathology laboratory information system (APLIS) alongside a digital pathology solution, laboratories not only stay ahead of the curve, but also ensure the highest standards of patient care and operational efficiency. APLIS integration facilitates the connectivity and automation that supports comprehensive workflow, advanced AI analysis, and enhanced patient safety. Centralized data management in the APLIS improves data integrity, security, and accessibility.
 Executive Summary
Executive Summary
- Digital pathology uses a whole slide imaging (WSI) scanner to digitize glass slides and analyze the digital images using an image viewer on a computer or mobile device.
- The rapid progression of WSI technology, advances in software applications, laboratory information system (LIS) integration, and high-speed data networks have enabled digital pathology to be fully integrated into workflows.
- Pathology labs use digital pathology for remote consultations, education, or quantitative analysis.
- With digital pathology, diagnosis is much faster because wait times for shipment of tissue samples are eliminated, and pathologists can review images remotely.
- Integration with a strong APLIS is necessary to achieve the full benefits that digital pathology has to offer.
- APLIS integration facilitates the connectivity and automation that supports a comprehensive workflow, advanced AI analysis, and enhanced patient safety.
 What is Digital Pathology?
What is Digital Pathology?
Digital pathology uses a WSI scanner to digitize glass slides and analyze the digital images using an image viewer on a computer or mobile device. Digital pathology encompasses the pathology workflow from slide scanning through visualization to analysis. Scanners can capture the glass slide image at a magnification comparable to a microscope. The image viewer works similarly to the microscope, allowing pathologists to zoom in and out and move slides. Digital slides can be shared across locations, and image analysis tools can assist in the interpretation.
Evolution of Digital Pathology
 The evolution of digital pathology has been going on for decades. More than 100 years ago, images were captured from a microscope onto photographic plates. The concept of transmitting microscopic images between locations — telepathology — has been around for nearly 50 years. Over that time, digital pathology evolved from simply attaching a camera to the microscope, to the development of the first scanners, to the digital pathology solutions we have today. Only in the last decade has digital pathology begun to take a strong root in healthcare. The rapid progression of WSI technology, advances in software applications, APLIS interfacing, and high-speed data networks have enabled full integration of digital pathology into workflows.
The evolution of digital pathology has been going on for decades. More than 100 years ago, images were captured from a microscope onto photographic plates. The concept of transmitting microscopic images between locations — telepathology — has been around for nearly 50 years. Over that time, digital pathology evolved from simply attaching a camera to the microscope, to the development of the first scanners, to the digital pathology solutions we have today. Only in the last decade has digital pathology begun to take a strong root in healthcare. The rapid progression of WSI technology, advances in software applications, APLIS interfacing, and high-speed data networks have enabled full integration of digital pathology into workflows.
 The first WSI system for digital pathology to be approved for primary diagnostic use by the U.S. Food and Drug Administration (FDA) was the Philips IntelliSite Pathology Solution (PIPS) in 2017. Though initially a slow progression, several other solutions have been granted FDA approval. More recently, in 2024, the Indica Labs HALO AP Dx Digital Pathology Platform and the Roche Digital Pathology Dx (VENTANA DP 200) received 510(k) clearance from the FDA.
The first WSI system for digital pathology to be approved for primary diagnostic use by the U.S. Food and Drug Administration (FDA) was the Philips IntelliSite Pathology Solution (PIPS) in 2017. Though initially a slow progression, several other solutions have been granted FDA approval. More recently, in 2024, the Indica Labs HALO AP Dx Digital Pathology Platform and the Roche Digital Pathology Dx (VENTANA DP 200) received 510(k) clearance from the FDA.
How is Digital Pathology Used?
Anatomic pathology labs use digital pathology for remote consultations, education, or quantitative analysis. Labs may use digital pathology powered by artificial intelligence (AI) to assign cases to pathologists, manage workflows, quantitate image analyses, integrate information into the LIS, and expand access to cases beyond the lab. AI applications can read a whole slide image and apply algorithms that can augment the role of the pathologist. Software applications can quantify aspects of tissue that may be impossible to see under a microscope to predict the patient diagnosis and outcome.²
Digital pathology is also used by large biopharmaceuticals and clinical research organizations for drug development processes in clinical trials. It is used for research (e.g., pharmaceutical companies, academic medical centers), study design, data collection, and database management.
Benefits of Digital Pathology
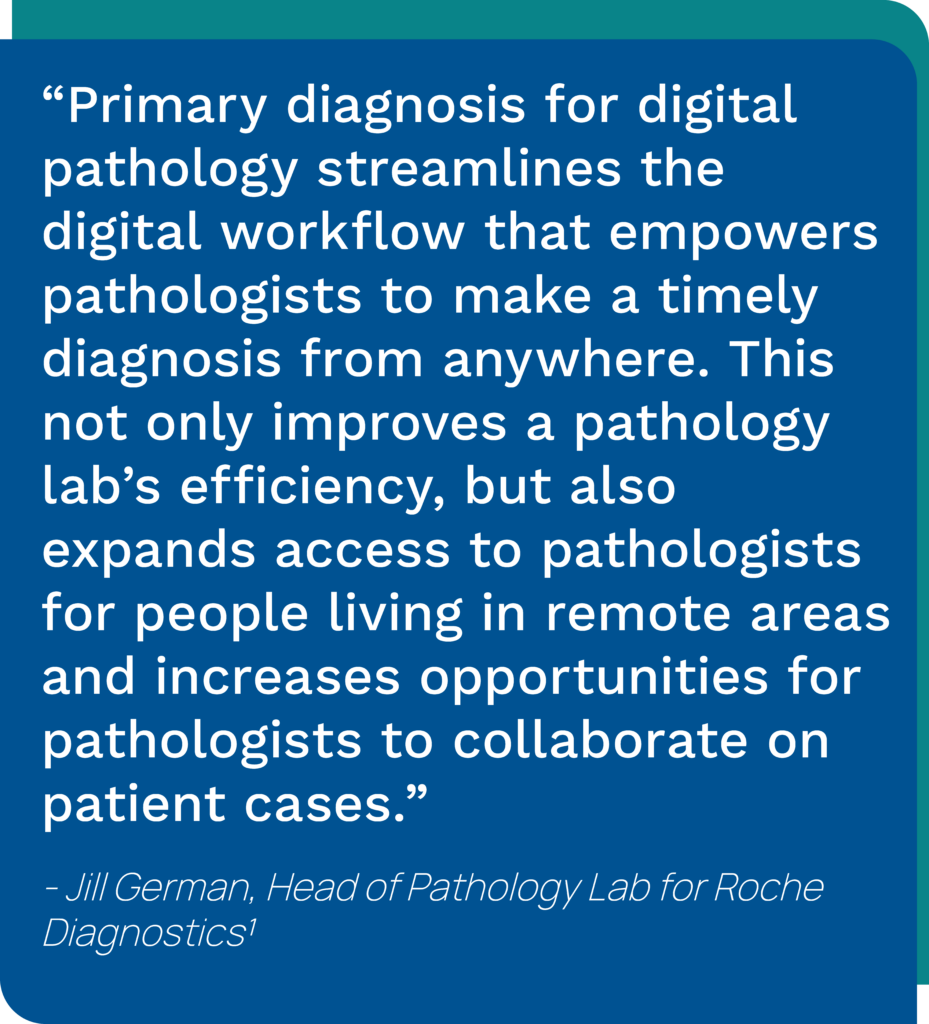
Digital pathology has brought about significant advancements in pathology lab efficiency. One of the biggest benefits of digital pathology is a boost in productivity because it can speed access to samples and improve turnaround time (TAT). With digital pathology, diagnosis is much faster because wait times for shipment of tissue samples are eliminated, and pathologists can review images remotely. In addition, digital pathology can improve slide analysis because analytic algorithms are objective, accurate, and faster than microscopy.
Digital pathology offers greater data security (digital slides cannot be lost or broken), easier slide access, sharing of cases, research standardization, and enables use of AI algorithms to improve diagnostic time and accuracy.²
Challenges & Barriers to Adoption
Even when pathologists realize that digital methods offer increased speed, accuracy, efficiency, and collaboration, implementation can seem daunting. Despite myriad benefits, significant challenges are associated with digital pathology, including cost, interoperability, and lack of reimbursement. In addition, pathologists’ resistance to change and adaptation has been a significant barrier.³
Cost
For many labs, cost is a major obstacle to implementing digital pathology technologies, particularly as laboratory budgets continue to shrink. Implementation of digital pathology requires significant investments for dedicated equipment and IT infrastructure. For example, the ability to zoom through large images can require upgrades to network equipment, application servers, and workstations. Achieving the appropriate field of view comparable to the microscope can require upgrades to higher-resolution monitors and 3D mice.
Reimbursement
Reimbursement also plays a major role in the slow adoption of digital pathology. In early 2024, the American Medical Association created several new digital pathology Category III add-on codes to measure staff work and service requirements associated with digitizing slides for primary diagnosis.⁴ These add-on codes are reported alongside primary pathology service codes and are not yet tied to reimbursement. They will be used to measure and audit the uptake of digital pathology solutions with the intent to associate reimbursement in the future. While this does not eliminate the upfront costs, it does help lay the groundwork for reimbursement and gives laboratories more confidence that the technology will be reimbursed.
FDA Clearance
The requirement in the United States for scanners to be FDA-approved has also slowed adoption, particularly in comparison to its adoption outside the U.S. The FDA-approved scanners from large manufacturers are also high-throughput instruments that are unnecessary for many smaller laboratories that could use a lower-throughput, less expensive scanner. Healthcare organizations that require the use of FDA-approved devices are more limited in their options for digital pathology implementation.⁵
Interoperability
To experience the benefits that digital pathology offers and track the technical component requires integration with an LIS that is pathology-focused. Integrating new digital pathology solutions with outdated LISs can be a struggle with minimal benefit. To further complicate the situation, some interoperability challenges are caused by the manufacturers themselves (e.g., creating images that cannot be read by other vendors’ viewers).
The Future of Digital Pathology Looks Promising
The declining number of pathologists combined with the rise in test volumes creates a demand for more efficient labs. Digital pathology is rapidly gaining momentum as a proven and essential technology. Its uses for education, research, development of AI and new molecular studies to predict cancer, as well as the practice of pathology are beneficial across the world. Digital pathology improves laboratory operational efficiency, productivity, and patient care.
Labs are overcoming obstacles to digital pathology implementation as more pathologists recognize the benefits and voice their preference for remote diagnostics. As more laboratories realize digital pathology’s benefits and take on the challenges of implementation, they are overcoming the hurdles of rearranging infrastructure. In addition, the adoption of digital pathology includes the benefit of AI image analysis that can move pathology forward. The outcome is faster, more accurate diagnoses and a broader volume of information readily available to treating providers.
Digital Pathology Success Stories
University of Michigan
Pathology informatics leaders at the University of Michigan are transitioning to a fully digital practice for primary diagnosis. They have implemented a new workflow within their histology lab, making Michigan Medicine the first in the U.S. to have radiology and pathology shared in the same picture archiving and communication system (PACS) and using the Digital Imaging and Communications in Medicine (DICOM) standard for workflow.⁶
Spectrum Healthcare Partners
Concerned about pathologist shortages in Maine and New Hampshire, the potential for digital pathology sign-outs from home encouraged retirement-age pathologists at Spectrum Healthcare Partners in South Portland, Maine to embrace digital pathology. The practice started providing digital pathology interpretations to its hospital clients in New England in December 2024, looking to use AI to enhance productivity and boost return on investment (ROI).⁷
Mayo Clinic
Mayo Clinic, in Rochester, Minnesota, continues its transition to digital pathology. As of January 2025, more than 50% of its surgical pathology cases, including 100% of dermatology cases, were being digitized and interpreted by pathologists via digital pathology. Mayo is planning to use AI to manage digitized cases and is developing algorithms for clinical diagnostics, such as breast and prostate cancer.⁸
 Pathology & Cytology Labs
Pathology & Cytology Labs
Pathology & Cytology Labs, in Lexington, Kentucky, is on the path to digital pathology implementation alongside Orchard® Enterprise Pathology™ APLIS. Driven by quality, P&C Labs anticipates their digital pathology-APLIS integration will boost their productivity and make the pathologists’ jobs easier, allowing them to innovatively continue to provide pathology care for the state of Kentucky. Their DP system improves productivity, saving time and money by eliminating logistic issues associated with case material transfer. With its digital imaging system, P&C Labs can augment their practice with expertise, logistics, and instant consultations.
APLIS Integration Enhances Digital Pathology Benefits
Successful pathology laboratories that are using digital pathology require a top-performing APLIS. The integration capabilities and tools within the APLIS enable pathology laboratories to gain the benefits that digital pathology provides.
Integration between the APLIS and digital pathology system elevates the laboratory’s diagnostic potential by enabling remote collaboration, improving TAT, patient safety, and supporting best patient care. This connectivity enables faster treatment decisions that lead to better patient outcomes and satisfaction. Leveraging AI algorithms and de-identified data, integration with a pathology-specific solution aids personalized care and precision medicine.
Interoperability Between the APLIS and Digital Pathology System is Crucial For Several Reasons:
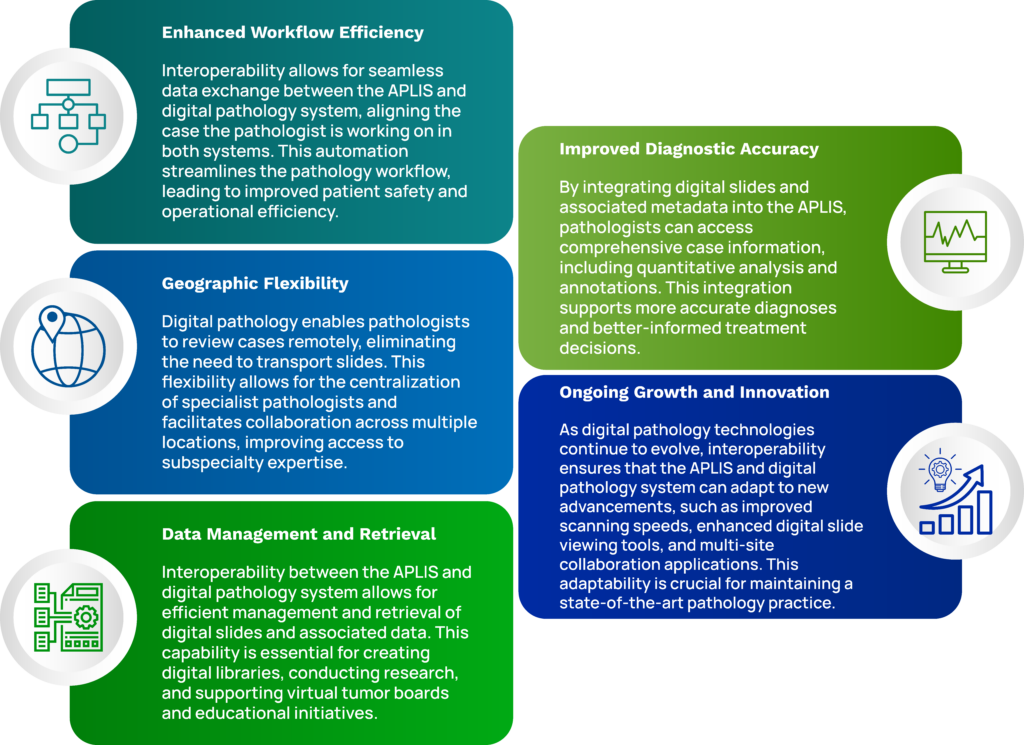
Overall, interoperability between APLIS and digital pathology systems is essential for optimizing pathology workflows, improving diagnostic accuracy, and enhancing the overall efficiency and quality of pathology services.⁹
Orchard Enterprise Pathology’s Digital Pathology Integration
Orchard Software’s digital pathology integration allows pathology laboratories to leverage the latest technologies to increase their diagnostic accuracy and geographical reach, enabling accelerated turnaround times and automated safety measures.
APLIS integration facilitates the connectivity and automation that supports comprehensive workflow, advanced AI analysis, and enhanced patient safety. Centralized data management improves data integrity, security, and accessibility.
By adopting Orchard Enterprise Pathology, Orchard’s pathology-specific LIS, alongside your digital pathology solution, your lab will not only stay ahead of the curve but also ensure the highest standards of patient care and operational efficiency.
References
- Roche Diagnostics. Roche receives FDA clearance on its digital pathology solution for diagnostic use. Published June 18, 2024. https://diagnostics.roche.com/us/en/news-listing/2024/rochereceives-fda-clearance-on-its-digital-pathology-solution-for-diagnostic-use.html.
- Jahn SW, Plass M, Moinfar F. Digital pathology: Advantages, limitations and emerging perspectives. J Clin Med. 2020 Nov 18;9(11):3697. doi: 10.3390/jcm9113697. PMID: 33217963; PMCID: PMC7698715. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7698715/.
- Schukow C, Allen T. Remote pathology practice: The time for remote diagnostic pathology in this digital era is now. Arch Pathol Lab Med. 2024;148(5):508–514. https://doi.org/10.5858/arpa.2023-0385-ED.
- College of American Pathologists. Digital pathology codes. https://www.cap.org/advocacy/payments-for-pathology-services/digital-pathology-codes.
- Ketchum K. Digital pathology use in labs growing, but barriers to adoption remain. 360dx. https://www.360dx.com/clinical-lab-management/digital-pathology-use-labs-growing-barriersadoption-remain. March 31, 2023.
- Paxton A. Department takes digital pathology to new level. CAP Today. January 2025.
- Klipp J, [Ed] Spectrum Healthcare Partners rolling out digital pathology services. Laboratory Economics. December 2024.
- Klipp J, [Ed] Lab execs share outlook for 2025. Laboratory Economics. January 2025.
- Ellin J, et al. Interoperability between anatomic pathology laboratory information systems and digital pathology systems. Digital Pathology Association. 2010.
