Today’s healthcare system is focused on care across the entire care continuum, including efforts to engage patients in care decisions, with the goal of proactively improving the health of the entire patient population. Population health management (PHM) programs are used to identify and improve the health of specific groups of patients. Using PHM, healthcare organizations (HCOs) can identify and understand their specific members’ diagnoses and needs, make appropriate interventions, and measure the effectiveness of outcomes.
Risk-stratifying Patients
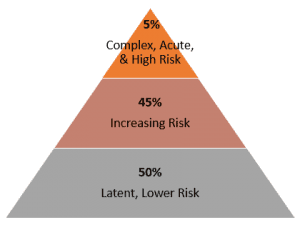 One of the crucial steps in PHM is accessing the patient data necessary to stratify patients into appropriate health categories. Think of the patient population divided into a pyramid. Depending on your healthcare facility type, typically the largest, bottom tier of the pyramid will be healthy patients who need preventive services depending on gender, age, etc. This “low-risk,” 50% of the population typically accounts for only about 8% of costs. The goal of a PHM program is to keep these patients healthy and in the low-risk category. The middle tier is “increasing-risk” patients who need care that keeps them from rising to the top tier. The top tier includes the sickest, “high-risk” patients with multiple co-morbidities. The high-risk tier is the costliest; typically, this 5% of patients accounts for about 50% of healthcare expenditures. Therefore, the high-risk tier is often a major target of a PHM plan. Patients in the high-risk category cost an average of 17 times more than patients in the lower-risk tier. Grouping patients into logical segments based on age, condition, risk, etc., allows providers and care teams to develop appropriate interventions for each group and each patient.
One of the crucial steps in PHM is accessing the patient data necessary to stratify patients into appropriate health categories. Think of the patient population divided into a pyramid. Depending on your healthcare facility type, typically the largest, bottom tier of the pyramid will be healthy patients who need preventive services depending on gender, age, etc. This “low-risk,” 50% of the population typically accounts for only about 8% of costs. The goal of a PHM program is to keep these patients healthy and in the low-risk category. The middle tier is “increasing-risk” patients who need care that keeps them from rising to the top tier. The top tier includes the sickest, “high-risk” patients with multiple co-morbidities. The high-risk tier is the costliest; typically, this 5% of patients accounts for about 50% of healthcare expenditures. Therefore, the high-risk tier is often a major target of a PHM plan. Patients in the high-risk category cost an average of 17 times more than patients in the lower-risk tier. Grouping patients into logical segments based on age, condition, risk, etc., allows providers and care teams to develop appropriate interventions for each group and each patient.
Chronic Disease Management
The sickest population of patients (though only 5%) accounts for the majority of healthcare spending. Therefore, management of chronic diseases is one of the most important functions of a PHM plan. Avoidable hospital admissions, unnecessary readmissions, and reducing hospital length of stay (LOS) add up to large savings. Certain conditions, such as diabetes, congestive heart failure, and COPD, are known to respond well to proactive interventions that can improve the patient’s quality of life and decrease costs. Laboratory data is used in part to identify patients in these high-risk groups because they are likely to benefit from additional interventions, creating an opportunity for providers and care managers to have a positive impact on outcomes.
Download the White Paper for More Details
To learn more to learn about how laboratory professional oversight of POCT can enhance POCT’s ability to positively impact patient engagement and outcomes, download Orchard’s white paper today.
Our Commitment
Orchard is committed to keeping you informed and being a trusted resource you can turn to for industry-related education. As always, we welcome your feedback. Follow us on Twitter at @OrchardSoftware, and feel free to respond to this post by emailing us at news@orchardsoft.com.
Notes
- Sullivan, P. (2015, May). 5 percent of Medicaid patients account for half of program’s costs. The Hill. Retrieved from http://thehill.com/policy/healthcare/241491-5-percent-of-medicaid-patients-account-for-50-percent-of-costs
- Stanton, M. W. (2006, June). The high concentration of U.S. health care expenditures. AHRQ Research in Action. Retrieved from https://archive.ahrq.gov/research/findings/factsheets/costs/expriach/
