 Executive Summary
Executive Summary
Together, anatomic and clinical pathology are the backbone of diagnostic medicine. Whether analyzing organ and tissue samples or bodily fluids, the specialty of pathology is at the heart of determining disease status. Being central to diagnostics, pathology has an exciting future. As our healthcare system continues to become more patient-centered and outcomes-based and new technologies are introduced, both clinical and anatomic pathology laboratories must adapt and find their place in the new healthcare paradigm. In addition, the SARS-CoV-2 pandemic brought long-lasting changes to our healthcare system that will continue to impact how we deliver care. However, as nothing in healthcare is simple, the changes that the pathology field is undergoing also come with challenges.
Key Takeaways
- Pathologists and the laboratories they oversee are looking for opportunities to show their value in the value-based healthcare arena.
- Pathology faces declining reimbursements, a greater focus on patient outcomes, and new technology developments.
- Developments in precision medicine and supporting technologies pave the way for pathologists to contribute in a more effective manner.
- Digital pathology and whole slide imaging (WSI) are widely considered to have the potential to completely transform the practice of diagnostic pathology.
- Experts predict that the true value of digital pathology will be realized as artificial intelligence (AI) methodologies gain in value and acceptance and are associated with digital imaging.
- To gain full benefit from WSI and employ a digital workflow, it is beneficial to integrate the anatomic pathology laboratory information system (APLIS) and the digital pathology System (DPS).
Pathology’s Shift from Volume to Value
Healthcare’s dynamic payment model shift from a focus on volume to one of value and improved patient outcomes is impacting every aspect of the medical field, and pathology is no exception. Pathologists and the laboratories they oversee are looking for opportunities to show their value in the value-based healthcare arena.
Currently, our healthcare system straddles a fee-for-service (FFS) payment model and various value-based models. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), on the value-based side, and the Protecting Access to Medicare Act of 2014 (PAMA), on the FFS side, are revamping the way pathology and clinical laboratory testing is reimbursed. The $1.4 trillion omnibus legislative package passed by Congress in December of 2020 reduced cuts that would have decreased Medicare reimbursements for pathology by 9% in 2021. Medicare professional component (PC) and technical component (TC) rates for most pathology services are expected to be cut by a few percent in 2022 according to the Proposed Medicare Physician Fee Schedule (MPFS).¹
Continued Industry Consolidation
These reimbursement cuts are part of the reason for widespread mergers and consolidations across laboratories and the entire healthcare industry. As a measure to achieve economy of scale, consolidation in healthcare continues to be a necessity. Specific to pathology, consolidation means more integrated pathology groups and laboratories that require greater health information technology (HIT) flexibility and functionality. In addition, some of the larger healthcare organizations that result from mergers and acquisitions are finding that they are more easily served and maintained with cloud computing. Consolidation could influence where pathologists are providing their professional services and push them to provide remote interpretations.
Rapid Deployment of New Tests & Advanced Technologies
 Pathology faces declining reimbursements, a shift to focus on quality outcomes, and new technology developments. How do pathology groups balance implementation of new technologies that improve productivity, efficiency, and accuracy while maintaining budget constraints?
Pathology faces declining reimbursements, a shift to focus on quality outcomes, and new technology developments. How do pathology groups balance implementation of new technologies that improve productivity, efficiency, and accuracy while maintaining budget constraints?
The practice of pathology is on the cusp of exciting new contributions as we advance in personalized medicine and move toward digital pathology. Developments in precision medicine and supporting technologies pave the way for pathologists to contribute in a more effective manner. Advances in molecular and genomic testing are allowing treatments to be more specifically tailored to individual patients. These developments alongside data processing advances are making it possible for pathologists to access and analyze more pathology-specific data.²
Digital pathology and WSI are widely considered to have the potential to completely transform the practice of diagnostic pathology. Having digitized slides paves the way for AI tools and machine learning (ML) algorithms to support pathologists in speedier, more accurate diagnosis and treatment planning.
Digital Pathology & WSI

While WSI is the digitization of a slide, digital pathology is a broader term that encompasses everything needed to incorporate those slides into a pathology workflow. As part of the shift to digital pathology, WSI is one of the first steps and is gaining traction among pathologists as a tool for diagnosis, education, and research. Slide digitization includes scanning, storing, editing, and displaying the slide image electronically. Images are scanned in a tile-by-tile manner and those individual tiles are put together to form an image of the entire slide. Slides are stored like a “pyramid” to allow the viewer to zoom in/out for greater/lesser magnification. The WSI process requires a specialized scanner to digitize the slides, hardware to digitize the slide image via scanning, a specialized slide viewer for review and analysis of the digitized image, algorithms to analyze the image data, and software to display the analyzed slide image and data to the pathologists. The image management system that accompanies WSI scanners allows slides to be annotated, and includes collaborative tools that enable digital sign-out, teaching, consultation, research, and quality assurance activities.
Myriad Uses for WSI
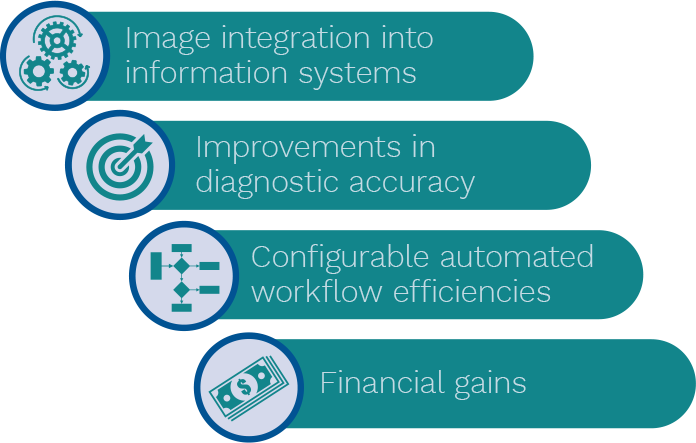 WSI has a plethora of clinical uses including telepathology, remote consultation, remote viewing of immunostains, slide display for tumor boards, and image analysis.³ Benefits in workload efficiency and balancing, and central clinical trial review are enabled by WSI. WSI is also of great value for educational and research purposes. Full implementation of WSI has positive potential, including improvements in diagnostic accuracy, workflow efficiency, image integration into information systems, and financial gains.³ WSI updates pathology workflows and allows pathology services to be provided in a more collaborative fashion. Digital technology can improve each stage of diagnosis from accessioning and grossing to analysis and reporting, including the ability to electronically share slides. As pathologists have always had an eye on quality and safety, digital pathology offers opportunities to improve both areas and boost efficiency at the same time.⁴
WSI has a plethora of clinical uses including telepathology, remote consultation, remote viewing of immunostains, slide display for tumor boards, and image analysis.³ Benefits in workload efficiency and balancing, and central clinical trial review are enabled by WSI. WSI is also of great value for educational and research purposes. Full implementation of WSI has positive potential, including improvements in diagnostic accuracy, workflow efficiency, image integration into information systems, and financial gains.³ WSI updates pathology workflows and allows pathology services to be provided in a more collaborative fashion. Digital technology can improve each stage of diagnosis from accessioning and grossing to analysis and reporting, including the ability to electronically share slides. As pathologists have always had an eye on quality and safety, digital pathology offers opportunities to improve both areas and boost efficiency at the same time.⁴
Barriers to Adoption

Yet, while the technology is available, its implementation is complex and challenging. One of the biggest hold-ups to greater adoption has been gaining FDA-clearance to use WSI for primary diagnosis. Long awaited, the Philips IntelliSite Pathology Solution gained approval in 2017 and the Leica Aperio Digital Pathology Solution was approved in 2019, confirming that use of digital images is not a quality concern.
Even with this step, the barriers to widespread adoption are significant. One barrier is the need to express the value of this technology to administrative leaders. When reimbursement is not immediately apparent, but rather a downstream improvement in workflow that improves productivity and patient care, it is more challenging to demonstrate ROI to healthcare administration.
In addition, the introduction of WSI requires specialized equipment and trained staff, a supporting IT system, and a pathologist workstation. This equipment can be an initial investment of around $200,000 plus ongoing support fees. According to Dr. Keith Kaplan, pathologist at Alliance Pathology Consultants, the average cost is about $1 per digitized slide, and the traditional glass slide is not eliminated.⁵
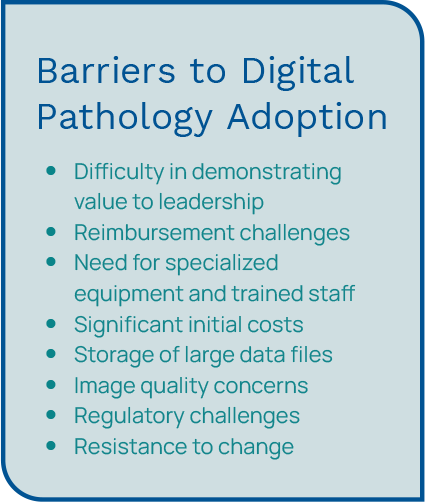 Another significant challenge is the size of the data files that are created. Even using file reduction techniques, a digitized slide can exceed a full GB, and therefore cannot easily be downloaded or displayed.⁶ With a single digital slide at two-to-five GBs, this qualifies as “big data” and significantly changes the way pathology is practiced.² Other barriers include problems with image quality and scanning certain materials, high costs, digital slide storage requirements, regulatory challenges, ergonomic concerns, and simple resistance to change.³, ⁴ Radical changes to a seasoned pathologist’s workflow can be challenging.
Another significant challenge is the size of the data files that are created. Even using file reduction techniques, a digitized slide can exceed a full GB, and therefore cannot easily be downloaded or displayed.⁶ With a single digital slide at two-to-five GBs, this qualifies as “big data” and significantly changes the way pathology is practiced.² Other barriers include problems with image quality and scanning certain materials, high costs, digital slide storage requirements, regulatory challenges, ergonomic concerns, and simple resistance to change.³, ⁴ Radical changes to a seasoned pathologist’s workflow can be challenging.
The Value Equation for Digital Pathology
The need for integration of molecular data and surgical and digital pathology into the electronic health record (EHR) has never been greater. Unless the value outweighs the costs, the implementation fails the cost-value equation. With healthcare dollars being closely scrutinized, fully implemented digital imaging can be a hard sell. Furthermore, to reap the full benefits of a digital workflow, there must be tight integration between all the instrumentation and information systems (e.g., slide scanner and reader, LIS, EHR, HIS, etc.).
The Pandemic as a Catalyst for Digital Pathology
Several driving factors have contributed to increased adoption of digital pathology during the COVID-19 pandemic. The pandemic forced pathologists to revisit the use of digital pathology, and as a result, the value of digital pathology and remote pathology services is becoming more accepted. The pandemic served as a catalyst for pathologists to adopt digital workflows and realize the advantages of these tools.
 For instance, many pathologists needed a way to work from home due to physical distancing guidelines. Digital pathology allowed pathologists to work from home and maintain quality patient care standards while minimizing the risk of COVID-19 exposure and preventing virus spread.⁷ Digital pathology platforms allow pathologists to view, analyze, share, and annotate digital slides from their home offices, eliminating delays in diagnosis and treatment during the pandemic.
For instance, many pathologists needed a way to work from home due to physical distancing guidelines. Digital pathology allowed pathologists to work from home and maintain quality patient care standards while minimizing the risk of COVID-19 exposure and preventing virus spread.⁷ Digital pathology platforms allow pathologists to view, analyze, share, and annotate digital slides from their home offices, eliminating delays in diagnosis and treatment during the pandemic.
The pandemic also moved certain legislation forward more rapidly. The Centers for Medicare and Medicaid Services (CMS) issued a waiver that allowed pathologists to work remotely. And the FDA relaxed some of its guidelines regarding the approval and validation of digital pathology–related technology to allow pathologists to work from home during the pandemic.
A study at The Ohio State University found that following the CMS waiver, 60% of pathologists reported using digital pathology for remote primary diagnosis, and 85.7% stated that they would continue to use these tools if restrictions were permanently lifted.⁸ In summary, COVID-19 accelerated acceptance of using digital pathology tools to allow pathologists to practice safely. However, there are still significant barriers to widespread adoption that need to be addressed.
AI on the Horizon
 There are those that predict that the true value of digital pathology will be realized as AI methodologies gain in value and acceptance and are associated with digital imaging. Big opportunities lie in using AI for diagnostic workups, particularly in guiding personalized cancer treatments. However, for pathologists to benefit from AI, they must have digitized slides as a starting point. Currently, there are several pathology-oriented AI tools (clinical decision-support algorithms) available to assist pathologists in reviewing cases. AI refers to computers that can “think” and learn and is quickly gaining traction in healthcare. ML is one type of AI that involves computers with the ability to develop models based on information received without any further programming or interventions. Specific to pathology, ML can aid in the discovery of patterns within images that can be used to make predictions. For example, ML algorithms are currently being used to help pathologists assess H&E stains used in the prognosis of breast cancer and lung carcinoma.⁶ AI tools can enhance digital imaging by providing a faster diagnosis and decreasing labor costs. These tools can augment the workflow of pathologists, aiding clinical decision support and enhancing care delivery. AI tools are expected to progress from supporting automated case review to computer-assisted diagnosis.⁶
There are those that predict that the true value of digital pathology will be realized as AI methodologies gain in value and acceptance and are associated with digital imaging. Big opportunities lie in using AI for diagnostic workups, particularly in guiding personalized cancer treatments. However, for pathologists to benefit from AI, they must have digitized slides as a starting point. Currently, there are several pathology-oriented AI tools (clinical decision-support algorithms) available to assist pathologists in reviewing cases. AI refers to computers that can “think” and learn and is quickly gaining traction in healthcare. ML is one type of AI that involves computers with the ability to develop models based on information received without any further programming or interventions. Specific to pathology, ML can aid in the discovery of patterns within images that can be used to make predictions. For example, ML algorithms are currently being used to help pathologists assess H&E stains used in the prognosis of breast cancer and lung carcinoma.⁶ AI tools can enhance digital imaging by providing a faster diagnosis and decreasing labor costs. These tools can augment the workflow of pathologists, aiding clinical decision support and enhancing care delivery. AI tools are expected to progress from supporting automated case review to computer-assisted diagnosis.⁶
Computers Handle Laborious, Repetitive Tasks
Pathologists must meticulously review extensive amounts of images to diagnose patients, sometimes examining hundreds of tissue slides for minute abnormalities. Pathologists can suffer from fatigue and eye strain as they scan images to detect these medical anomalies. Because of these types of repetitive tasks, pathology is a specialty ripe to benefit from properly integrated AI tools. AI tools can easily perform laborious and mundane tasks without tiring or losing concentration. AI has the power to take over certain tasks where computers outperform humans, particularly in image-rich fields, such as pathology and radiology. It is logical that digital technologies can be used for repetitive tasks that have higher observer variability, such as estimating the percentage of tumor cells in a lung cancer patient.⁴ AI algorithms can review every inch or pixel of a digital slide with a higher tumor-level sensitivity and comparable performance levels to a pathologist. Because AI tools are “trained” with enormous amounts of data, these systems can often provide more accurate diagnoses than a human for routine diagnostics.⁹
Leveraging the Human-Computer Workload Balance
The idea behind using AI in conjunction with digital images is to reduce the time pathologists spend on time-consuming, mundane slide analysis, allowing their focus to be on tasks that require human processing. Medicine must find that balance between assigning computers the tasks that computers perform best and saving specific tasks that need a human’s way of thinking for the clinicians. Having this powerful combination of human and machine thinking gains better results than either alone. Of note, less than 2% of medical students choose pathology as a specialty. AI tools can help alleviate the pathologist shortage and reduce the workload burden on those currently practicing.⁹
Successful AI Examples in Pathology
 ML and deep-learning algorithms can aid pathologists’ decision-making by allowing them to review large amounts of detailed data with computer-level accuracy. In one example at Case Western Reserve University, a deep-learning network was used to correctly identify breast cancer in pathology images 100% of the time.¹⁰ In precision medicine efforts, a study at Stanford University School of Medicine used ML to accurately identify two types of lung cancers.11 Having the ability to assess a tumor and gain an understanding of whether a patient will respond to a specific therapy using an AI tool and digital imaging is incredibly valuable.
ML and deep-learning algorithms can aid pathologists’ decision-making by allowing them to review large amounts of detailed data with computer-level accuracy. In one example at Case Western Reserve University, a deep-learning network was used to correctly identify breast cancer in pathology images 100% of the time.¹⁰ In precision medicine efforts, a study at Stanford University School of Medicine used ML to accurately identify two types of lung cancers.11 Having the ability to assess a tumor and gain an understanding of whether a patient will respond to a specific therapy using an AI tool and digital imaging is incredibly valuable.
At The Ohio State University Comprehensive Cancer Center, they use digital images as part of their routine diagnostic workflow and have determined that due to increased productivity and error reduction, implementation of their digital pathology system will pay for itself in five years.⁸
Information_Systems_and_Digital_Pathology_Systems.pdf
They are leveraging their digitized images to use alongside an AI tool for repetitive tasks, such as identifying metastases in lymph nodes, grading cancers, and developing biomarker detection tools to help determine which patients will benefit from a particular drug.⁸
In another example of an AI tool effectively being used in pathology, Google has developed a deep-learning algorithm called LYmph Node Assistant (LYNA) that improves both speed to diagnosis and accuracy in detection of metastatic breast cancer.12 These AI tools can tirelessly review every section of a digital image, effectively reducing the workload of pathologists and assisting with case triage.
The FDA recently approved an AI software to assist in prostate biopsy review. As an adjunct-to-pathologist review of digitized prostate biopsy images, Paige Prostate identifies areas of interest on the images that contain the highest likelihood of cancer for further review. This AI tool is designed to aid pathologists in the best initial diagnosis.13
While these are exciting endeavors, there are still hurdles ahead before AI technologies are widely used. Implementing digital imaging and AI tools so that they function well in daily practice is likely to be quite some time away. To gain buy-in from pathologists, AI tools need to be easy to use, trustworthy, and show a financial gain.
Informatics & Clinical Decision-making
With this expanse of growing technology, today’s pathologists must be able to gather different pieces of information from various tests and sources and use that data alongside the clinical picture to support clinical decision-making. It has been posited that in the future, radiologists and pathologists may merge into a new role as information specialists whose job will be managing the information that AI extracts from images and associating it with the patient’s clinical picture.¹³ The need to analyze, interpret, and store large data sets is already changing the way pathologists practice, and pathology informatics is quickly gaining as a much needed subdiscipline.
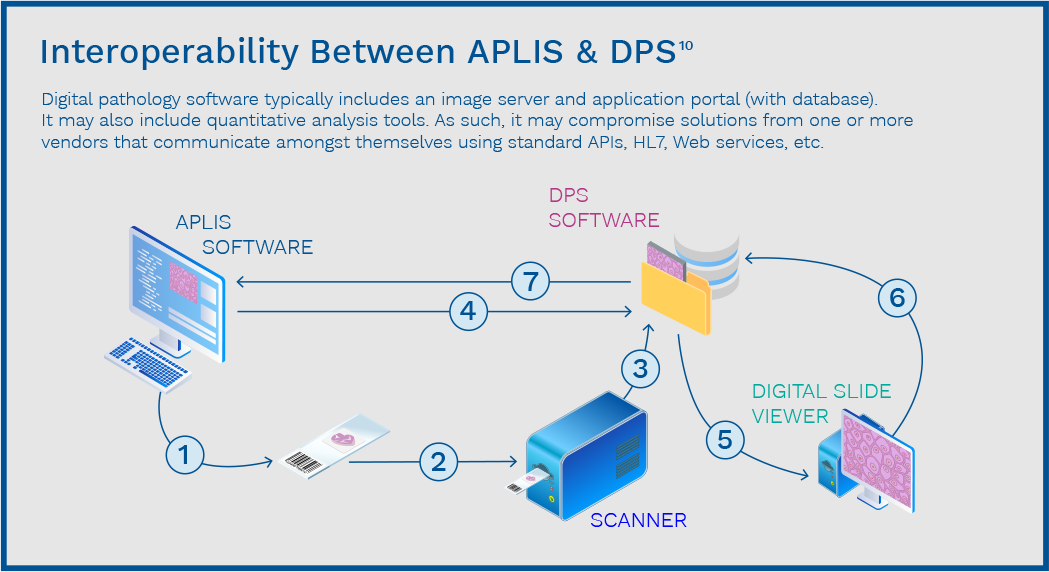
The APLIS & DPS Integration
Adoption of digital pathology ideally requires integration with an APLIS. In this scenario, the APLIS helps manage the pathology workflow, handling worksheets, specimen tracking, reporting, and aiding in proper coding and billing. The DPS has been developed to manage WSI and is like the picture archiving and communication system (PACS) used in radiology. The DPS can create and store the WSI where pathologists can access, view, share, and annotate the images. To fully embrace WSI and employ a digital workflow, it is beneficial to integrate the APLIS and the DPS.15

About Orchard Enterprise Pathology
Orchard Enterprise Pathology is an inherent diagnostic solution within Orchard Enterprise Lab that allows pathology laboratories to implement automated workflows and electronic worksheets that drive efficiency and patient safety. Sophisticated decision-support rules and data mining capabilities allow standardization of processes, synoptic reporting, and tracking of key performance indicators. Orchard’s expertise in integration and interfacing supports organizational interoperability and data sharing to promote patient-centered care. Orchard’s enterprise-level solution allows laboratories to function efficiently, safely, and profitably—positioning healthcare organizations for ultimate security, reliability, growth, and success. With the addition of Orchard Enterprise Pathology, our customers can scale their laboratory informatics to meet their business growth needs and ultimately provide better patient care.
 Orchard® Enterprise Pathology™
Orchard® Enterprise Pathology™
Expertly Address Today’s Pathology Challenges & Prepare Your Lab for the Future
Orchard Enterprise Pathology is a web-based laboratory information system designed to enable pathology laboratories to continue to grow, adapt to healthcare changes, and be an integral part of an interoperable system.
References
- Klipp, J. [Ed.]. Medicare Rates For Pathology Services To Get Nicked. Laboratory Economics. Vol. 16. No. 8. August 2021.
- Gu, J., Taylor, C.R., & Phil, D. Practicing pathology in the era of big data and personalized medicine. Appl Immunohistochem Mol Morphol. 2014; 22(1): 1-9. doi: 10.1097/PAI.0000000000000022
- Farahani, N., Parwani, A., & Pantanowitz, L. Whole slide imaging in pathology: Advantages, limitations, and emerging perspectives. DovePress. 2015; 7: 23-33. https://doi.org/10.2147/PLMI.S59826
- Griffin, J. & Treanor, D. Digital pathology in clinical use: Where are we now and what is holding us back? Histopathology. 2017; 70 (1): 134-145. https://doi.org/10.1111/his.12993
- Klipp, J. [Ed.]. How Much Longer Until Digital Pathology Takes Off? Laboratory Economics. Vol. 16. No. 4. April 2021.
- Zarella, M.D., Bowman, D., Aeffner, F., et al. A practical guide to whole slide imaging: A white paper from the digital pathology association. Archives of Pathology & Laboratory Medicine. 2019; 143 (2): 222-234. https://doi.org/10.5858/arpa.2018-0343-RA
- Browning, L., Colling, R., Rakha, E., et al. Digital pathology and artificial intelligence will be key to supporting clinical and academic cellular pathology through COVID-19 and future crises: The PathLAKE consortium perspective. J Clin Pathol. 2020:1-5. doi:10.1136/jclinpath-2020-206854
- Lujan, G.M., Savage, J., Shana’ah, A., et. al. Digital Pathology Initiatives and Experience of a Large Academic Institution During the Coronavirus Disease 2019 (COVID-19) Pandemic. Arch Pathol Lab Med. May 2021, 145 (9): 1051–1061. https://doi.org/10.5858/arpa.2020-0715-SA
- Dolgin, E. The first frontier for medical AI is the pathology lab. IEEE Spectrum. 2018. https://spectrum.ieee.org/biomedical/diagnostics/the-first-frontier-for medical-ai-is-the-pathology-lab
- Ellin, J., Haskvitz, A., Premraj, P.; Shields, K., Smith, M.; Stratman, C., Wrenn, M. Interoperability between Anatomic Pathology Laboratory Information Systems and Digital Pathology Systems. Digital Pathology Association. October 2010. https://digitalpathologyassociation.org/_data/cms_files/files/Interoperability_Between_Anatomic_Pathology_Laboratory_Information_Systems_and_Digital_Pathology_Systems.pdf
- Kent, J. How artificial intelligence is changing radiology, pathology. Health IT Analytics. 2018. https://healthitanalytics.com/news/how-artificial-intelligence-is-changing-radiology-pathology
- Stone, J. Studies show potential for Google’s AI tools to improve pathologist accuracy and efficiency. Dark Daily. 2018. https://www.darkdaily.com/studies-show-potential-for-googles-ai-tools-to-improvepathologist-accuracy-and-efficiency/
- Ridley, E., L. FDA clears 1st prostate pathology AI software application. LabPulse.com. September 2021. Accessed at: http://www.labpulse.com/index.aspxsec=nws&sub=rad&pag=dis&itemid=802302
- Jha, S. & Topol, E. Adapting to artificial intelligence: Radiologists and pathologists as information specialists. JAMA. 2016. doi:10.1001/jama.2016.17438
- Guo, H., Birsa, J., Farahani, N., et al. Digital pathology and anatomic pathology laboratory information system integration to support digital pathology sign out. J Pathol Inform. 2016; 7:23. doi:10.4103/2153-3539.18176

